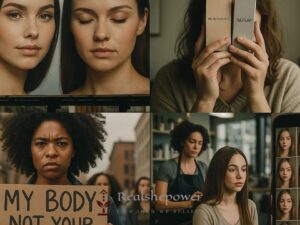
Life changes dramatically when a newborn enters your world. There’s the intense joy and unconditional love that fills your heart. But for some mothers, this monumental life event is also accompanied by something unexpected – postpartum depression (PPD). It’s an important topic that needs addressing, so let’s embark on a detailed exploration of postpartum depression, its symptoms, and the treatment options available.
Table of Contents
Postpartum Depression: What Is It?
Postpartum depression, also known as PPD, is a type of mood disorder associated with childbirth. It can affect both sexes but is most commonly experienced by women. The American Psychological Association (APA) states that one in seven women might experience PPD, making it a significant public health concern.
The term ‘postpartum’ refers to the period following childbirth. The “baby blues,” a common experience involving mood swings, anxiety, and trouble sleeping, typically occurs soon after delivery and lasts for a few days. Postpartum depression, on the other hand, is far more intense and can persist for months or longer. It usually appears within the first few weeks after childbirth, but symptoms can emerge anytime within the first year.
Recognizing the Symptoms of Postpartum Depression
The symptoms of PPD often mirror those of major depression, and they can range from mild to severe. It’s important to remember that every individual’s experience is unique, but common symptoms can include:
Feelings of sadness, hopelessness, or being overwhelmed
Crying more often than usual or for no apparent reason
Trouble sleeping (insomnia) or sleeping too much
Eating too little or too much
Trouble concentrating, remembering details, or making decisions
Experiencing anger or rage
Losing interest in activities you used to enjoy
Withdrawing from friends and family
Suffering from physical aches and pains, including frequent headaches, stomach issues, and muscle pain
Having thoughts of harming yourself or your baby
Questioning your ability to care for your baby
Risk Factors for Postpartum Depression
Certain factors can increase the risk of developing PPD. However, it’s crucial to note that having these risk factors does not guarantee that PPD will occur. It simply means the chances are higher. These factors can include:
A history of depression or other mental health disorders
A family history of depression or mental health disorders
Experiencing stressful events during the past year, such as pregnancy complications, illness, or job loss
Mixed feelings about the pregnancy, whether it was planned or unplanned
Being a first-time mother
Having a lack of strong emotional support from family and friends
Experiencing financial problems
Postpartum Depression: When to Seek Help
Recognizing the signs of PPD is the first step toward recovery. If you suspect you’re experiencing postpartum depression, it’s vital to seek help promptly. Remember that PPD is not a weakness or something to be ashamed of – it’s a medical condition that requires professional help.
If you or someone close to you exhibits symptoms of PPD, reach out to a healthcare professional. If there’s an immediate concern about your safety or the safety of your child, it’s critical to get help right away. Reach out to a mental health crisis hotline or go to the emergency room. You’re not alone, and help is available.
Treatment Options for Postpartum Depression
The good news is that postpartum depression is treatable, and a range of options is available. The best approach often involves a combination of treatments, including:
Psychotherapy: Also known as talk therapy or counseling, this treatment involves talking about your thoughts with a mental health professional. Cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT) have been particularly effective for treating PPD.
Medication: Your doctor might recommend antidepressants. These medicines can help manage the symptoms of PPD. If you’re nursing, it’s important to discuss this with your healthcare provider as some medications can enter breast milk.
Hormone therapy: If your PPD is thought to be related to the drastic drop in estrogen following childbirth, hormone therapy might be recommended.
Lifestyle changes: Regular physical activity and a healthy diet can boost your mood and energy levels. Aim to get adequate sleep, take time for yourself, and avoid alcohol, caffeine, and processed foods.
The Road to Recovery
Recovery from postpartum depression takes time and patience. It’s essential to remember that it’s OK to ask for help, whether it’s professional help for the treatment of PPD or simply asking a friend or loved one to help with baby care or household chores.
Having postpartum depression does not make you a bad parent. It does not mean you don’t love your child. It simply means you’re dealing with a significant health issue that needs attention.
If you’re a loved one of someone dealing with PPD, your support can make a tremendous difference. Encourage them to speak about their feelings, accompany them to appointments, and offer help with their day-to-day tasks.
In Conclusion
Understanding postpartum depression is the first step to managing it. Recognize that it’s a common and treatable condition. If you or a loved one is suffering, don’t hesitate to reach out to healthcare professionals. Remember, it’s not a sign of weakness to seek help. It’s a sign of strength.
With awareness, understanding, and the right treatment, postpartum depression can be overcome. And remember, it’s okay not to be okay. You’re not alone. Help is available, and it’s okay to ask for it.

Sparnod Fitness STH‑3002 Home Walking Pad Treadmill
Ultra‑slim, compact, and ready to use—no assembly needed. 2.5 HP motor, 1‑6 km/h speed, 2‑level incline, shock absorption, LED display, rolls under bed.
👉 View on Amazon